Brian Klepper
 The attached PP deck is a presentation I’ve given several times that has received an overwhelmingly positive, if frightened, reception.
The attached PP deck is a presentation I’ve given several times that has received an overwhelmingly positive, if frightened, reception.
It is, perhaps, the most disturbing public argument of my career (which is going some), because it tries to document the health care industry’s “capture” of health care regulatory processes, particularly those that govern payment. The result, as many people understand, is that the health care industry, in its rapaciousness, is effectively driving the larger US economy off a cliff.
Only one group, the non-health care business community, has the heft, influence and motivation to save us, though health care has done a good job dividing and conquering this sector as well, insinuating itself into many of the most powerful institutions (e.g., the Chambers of Commerce). It remains very unclear that the business community can be galvanized/mobilized from its malaise to turn this problem around.
The argument goes like this:
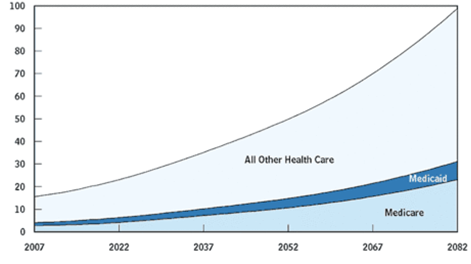
- The data are clear that the US’ health care economy is absorbing most gains in the larger economy, and driving the US economy toward collapse. For example, nearly all increases in total compensation have been directed at increasing health costs, which in turn flows into the health industry.
- Reasonable estimates of health care wasteshow that half or more of all current health care expenditures, or currently about $1.5 trillion each year, provide no value. To put this into perspective, remember that the Congressional Super-Committee sought $1.2 trillion over ten years. (They failed.)
- Continue reading “Why Only Non-Health Care Business Can Save America From The Health Care Industry”





 In this post, we will examine what we and many other commentators view as inevitable: the demise of volume-based payment systems and how the drive for greater value will cause physicians and insurers re-examine their normally antagonistic relationship.
In this post, we will examine what we and many other commentators view as inevitable: the demise of volume-based payment systems and how the drive for greater value will cause physicians and insurers re-examine their normally antagonistic relationship.
